Carsten Tschöpe
At the 2019 European Society of Cardiology (ESC) Congress (31 August–4 September, Paris, France), Carsten Tschöpe (Charité Hospital, Berlin, Germany) outlined the use of the “Propella” approach in myocarditis patients with cardiogenic shock. He explained that the approach involves the prolonged use of an Impella heart pump (Abiomed) to provide circulatory support and, potentially, disease modifying effects. He noted that such a Propella approach could, potentially, be used as a “bridge to recovery” in patients with cardiogenic shock.
According to Tschöpe, myocarditis is “very often not a big deal” but can be severe in some patients and can cause cardiogenic shock—at least 20% of patients with myocarditis will develop “the shock scenario” and require circulatory support. There are several such circulatory support systems available, but extracorporeal membrane oxygenation (ECMO) is used to treat the majority of patients. However, although ECMO does provide circulatory support, it can cause stress to the heart because it increases after-load and, consequently, also enhances oxidative stress. Tschöpe commented: “This, in an inflammatory situation, is extremely undesirable.”
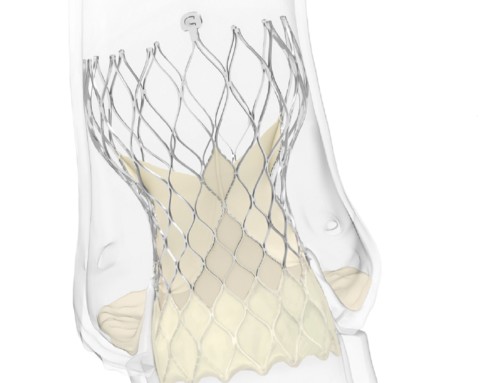
In an interview with Cardiovascular News, Tschöpe said: “Like with ECMO, the Impella device also provides circulatory support, but [when using an Impella device] the heart is unloaded. The Impella, which is implanted in the left ventricle, acts like a propeller in a boat. It swaps the blood out, so the heart does not have to pump. This reduces the volume load, and therefore reduces the stress for the heart.” He added that the device does not come into contact with the venous system. By contrast with veno-arterio (VA) ECMO, the venous blood leaves the heart from the right ventricle, passes through the oxygenator, and then enters the heart through the arterial system, against the direction of blood flow in the organ. “So [with ECMO] you have no unloading, meaning you are not relieving the pressure for the heart,” Tschöpe clarified.
Therefore, nearly two years ago, Tschöpe and colleagues set out to determine if myocarditis patients with cardiogenic shock would benefit from an unloading approach using the Impella device rather than using ECMO.
They hypothesised that unloading, especially in severe myocarditis, would provide extra benefits to circulation support. “In some scenarios ECMO is extremely important and necessary”, Tschöpe explained, “but I believe that when the right ventricular function is fine, the unloading is the better approach because in addition to stabilising the circulation, you are doing something in addition to address the inflammation of the heart.” He likened the effects of unloading to a “cast” for the heart—allowing the organ to rest.
Furthermore, while ECMO device can only be implanted for 10 days, the Impella device is not beholden to such a narrow timeframe. With ECMO, the patient is intubated and unable to get out of bed. After 10 days, the risk of complications—such as bleeding and infections—increases. “It is a really dangerous scenario”, Tschöpe stated. With Impella, however, a patient is able to get up and walk around while in hospital, when implanted via the axillary. This lowers the risk of complications and, consequently, allows for prolonged unloading with the device, giving more time for the heart to heal. The prolonged use of Impellla, or Propella for short, can extend implantation to 28 days. “Some of these pumps are functional up to 50 days, or even longer”, Tschöpe commented. Additionally, the extended window also allows more time for anti-inflammatory drugs (to treat the myocarditis) to take effect.
In his talk at the ESC, Tschöpe outline a case in which a young man with severe biopsy-proven myocarditis who although was not in cardiogenic shock, was not showing signs of recovery. Therefore, Tschöpe and his colleagues implanted an Impella device. “It did exactly what we expected”, he said. Monitoring the pressure-volume of the heart over time demonstrated that there was successful unloading. After two weeks of the patient being on steroids and the Impella device, an echo showed poor left ventricular function—indicative of no recovery. However, 10 seconds after stopping the Impella function, Tschöpe and colleagues witnessed the left ventricule starting to pump. “For me”, Tschöpe said of this observation, “that was the most impressive thing. This was a form of self-controlled, Impella-induced, unloading-induced hibernating”.
The Propella technique is “sufficient to overcome the inflammatory process”, Tschöpe explained. Analysing the protein profile of biopsies taken two weeks after Impella implantation revealed an improvement in Titin phosphorylation, energy metabolism, and collagen expression. The number of inflammatory cells decreased. Expression of mRNA coding for the mechanoreceptor integrin reduced during unloading, but, when the researchers removed the pump, levels increased to normal. “This makes sense because without the pump, you can increase integrin without the unloading consequences,” Tschöpe said.
“The concept here is that behind circulatory support, uncontrolled loading induces remodelling as well as inflammatory systems, which further decreases the functional prognosis of patients. We see that with the Propella approach, in addition to the mechanical unloading, we also get this molecular unloading, which is extremely important for the prognosis of the patient.”
Earlier this, Tschöpe and colleagues published the results of their experience with using the Impella device in the European Heart Journal. In that paper, they concluded that the Propella approach “may provide benefits beyond its primary function of mechanical circulatory support in the form of additional disease-altering effects, which may contribute to enhanced myocardial recovery/remission in patients with chronic fulminant myocarditis”.