V-Lap
A clinical trial, being conducted at the Queen Elizabeth Hospital (Birmingham, UK), of the world’s first wireless in-heart microcomputer has begun. A press release reports that researchers hope that the ground-breaking technology will dramatically improve the quality of life for people living with heart failure, helping them better manage the condition and prevent the need for admissions to hospital.
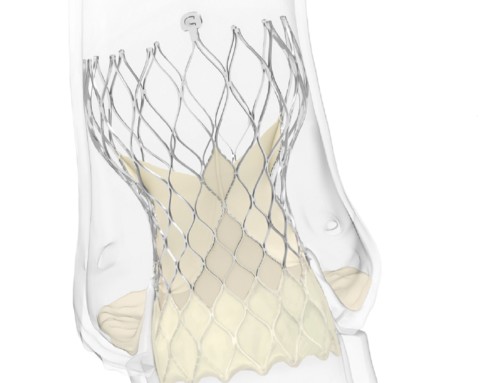
The device (V-LAP, Vectorious) is implanted in the left atrium and is designed to give the earliest, most accurate data of the heart’s performance. Its sensor does not have a battery, which means it potentially could last for all of the patient’s life. It is charged remotely from outside the patient’s body, feeding back data to doctors as it does so.
According to a press release, the minimally-invasive procedure to implant the device is a low risk one and is completed in less than an hour. In normal use, patients are able to return home the same day after the operation. The data provided by the device is analysed by artificial intelligence and machine learning will be used to provide doctors with information to help them intervene early, to detect important events and help patients remain well balanced medically and safe.
Vectorious hope that by providing regular data, rather than relying on the current assumptions based on physical findings, doctors will be able to help patients actively manage their conditions and reduce the need for them to be admitted to hospital. This will not only improve the quality of life for the patient, but also enable cost savings for healthcare services.
Francisco Leyva (Queen Elizabeth Hospital, Birmingham, UK), says: “This new device has the potential to combat three of the biggest problems relating to heart failure disease; low patient quality of life, repeat admissions to hospital and the astronomical cost to the healthcare system of readmissions. Today, physicians base the treatment of heart failure on external signs and symptoms such as shortness of breath and gaining weight—which appear at a late stage, so the patient does not get the medication they need to stable their condition early enough. 44% of patients are re-hospitalised within a year from the first acute event, so this device shows real promise in reducing those readmissions, and the costs associated.”