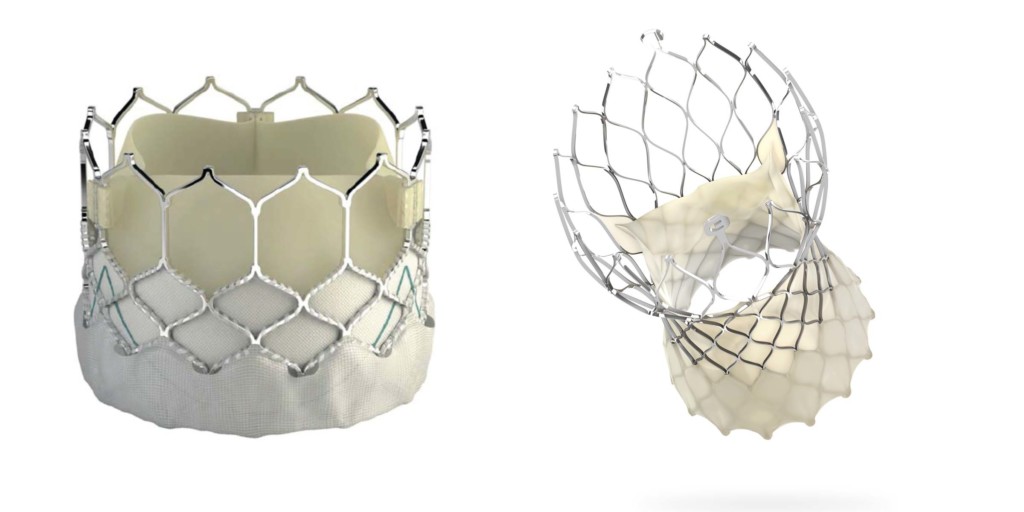
Sapien 3 and CoreValve Evolut Pro
According to two studies published in Circulation, the balloon-expandable Sapien (Edwards Lifesciences) transcatheter aortic valve implantation (TAVI) system is associated with lower mortality than is the self-expanding CoreValve (Medtronic) system. These findings have led to calls for randomised head-to-head trials comparing the two devices.
In their paper, Eric Van Belle (Department of Cardiology, Institut Coeur Poumon, Centre Hospitalier Universitaire de Lille, Lille, France) and others report that “despite major differences” between balloon-expandable and self-expanding valves, the devices “are recommended to be used indifferently in most of the clinical situations”. They add that whether these valves achieve similar or different clinical outcomes “remains unclear”, noting that a large randomised study powered to compare the two devices has not been performed (or initiated) even though “there is an urgent clinical need to clarify this issue in an exponentially growing therapeutic field”.
Therefore, to provide further information in this area, Van Belle et al conducted a retrospective review of outcomes for patients (12,141) enrolled in the France-TAVI registry patients who underwent TAVI in France between 2013 and 2015. Of these patients, they identified 3,910 matched pairs. The first co-primary outcome of the study was assessment of paravalvular regurgitation at discharge and the second co-primary outcome was two-year all-cause mortality.
The authors report that more than mild paravalvular regurgitation was more frequent in patients who underwent TAVI with CoreValve: 15.5% vs. 8.3% for Sapien. All-cause mortality, at two years, was also higher in the CoreValve patients: 899 of 3,910 patients vs. 801 of 3,910 patients. They add: “when only cardiovascular mortality was considered, self-expanding transcatheter heart valves remained associated with higher short-term mortality.” However, Van Belle et al observe that—for all-cause mortality—proportional hazard assumption was not satisfied as the excess mortality risk of CoreValve compared with Sapien was only seen for the first three months.
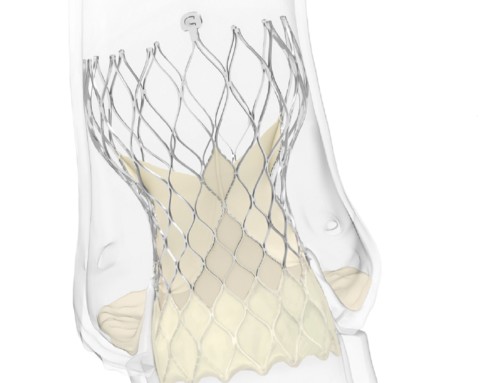
Of note, the registry did include patients who received older generation devices but, according to the authors, the results were similar when their review was restricted to after newer iterations (post 2014) of the valves were introduced. They comment that while Sapien 3 (the latest generation of Sapien included in the study) has a “anti-leak skirt” that has been associated with reduced paravalvular leak, the newer generations of CoreValve that were included in the study have not been associated with similar reductions. “Whether the newest iteration of the self-expanding transcatheter heart valve (Evolut Pro) featuring an outer pericardial wrap will achieve to mitigate this major difference is unknown. A recent small non-randomised comparison did not show a significant difference in paravalvular regurgitatio rates between the last two iterations of self-expanding transcatheter heart valves (Evolut vs. Evolut Pro),” Van Belle et al say.
The second paper in Circulation to compare outcomes with Sapien with those of CoreValve also reviewed outcomes of patients who underwent TAVI in France. However, authors Pierre Dehara (Department de Cardiologie, CHU Timone, Marseille, France) and others restricted their review to patients who received TAVI after 2014 (to June 2019); therefore, only looked at later generation TAVI valves (Sapien 3, CoreValve Evolut R, and CoreValve Evolut Pro).
In their study, they identified 10,459 matched pairs. At a mean follow-up of 358 days, all-cause death was lower in the Sapien group: 14.4% a year vs. 16.4% for the CoreValve group. Cardiovascular death and risk of hospitalisation for heart failure were also lower in the Sapien group, meaning that the rate of the combined endpoint of all-cause death, all-cause stroke, or rehospitalisation for heart failure was lower with Sapien. Pacemaker implantation during the first 30-days after TAVI was again lower with Sapien.
Dehara et al comment their findings “underscore the need for large-scale dedicated randomised trials on this issue [how balloon-expandable valves compare with self-expanding valves]”. Similarly, Van Belle et al conclude: “As some of the most recent transcatheter heart valve iterations were not part of the investigation, there is an urgent need to conduct a randomised trial sufficiently powered to compare head-to-head the latest generation of self-expanding and balloon-expandable transcatheter heart valves on all-cause mortality.”

Mohamed Abdel-Wahab
However, a randomised head-to-head trial—at least, not one supported by industry—may not happen. Mohamed Abdel-Wahab (Department of Internal Medicine/Cardiology, Heart Center Leipzig, University of Leipzig, Leipzig, Germany), who wrote a commentary about the studies in Circulation, told BIBA Briefings that “unfortunately, companies are not interested in initiating such a trial”.
He does think that the results do need to be confirmed in randomised trials and, at present, should be interpreted with “great caution”. “Despite the sophisticated statistical adjustment the most reasonable cause for the difference in mortality is residual confounding. However, one might speculate that the less occurrence of paravalvular leak and the less need for pacemakers with balloon-expandable valves do impact mortality as well; though this needs to be confirmed in a randomised setting,” he says. Abdel-Wahab adds that while there is an “unequivocal” association between paravalvular leak and mortality, “causality has never been proven”. He notes “The problem of paravalvular leak remains in its assessment. More than mild forms are clearly associated with mortality, but this is less evident for mild forms, which probably need a more granular classification system”.
In his commentary, which he co-wrote with Holger Thiele (also Leipzig, Germany), he states that anatomy and experience are the most relevant factors for device selection but neither can be entirely corrected for in analyses such as the two studies. “Experience being quite unmeasurable (despite the authors’ attempts) and anatomical data (based on sophisticated computed tomography measurements) being unavailable”, Abdel-Wahab and Thiele state. Dehara et al also make the point that future research is needed to address whether anatomical features (and certain baseline characteristics) may favour one TAVI technology over another. Abdel-Wahab explains that although both device types can probably perform in a similar way in “a large percentage of patients”, short valves—such as balloon-expandable ones—may be preferable in “patients with coronary disease (allowing easier access), younger patients with expected longevity and redo procedures (probably easier to retreat), and those with large anatomies (more radial force and less leaks)”. He adds: “Supra-annular self-expanding devices are preferred in small anatomies and for valve-in-valve procedures because of their superior haemodynamics”.
Whether or not a head-to-head randomised trial of balloon-expandable valves vs. self-expandable valves is performed, Abdel-Wahab does not think one established TAVI valve should be used as the comparator for all pivotal trials of novel devices. He says a “more sound” approach would be to compare new balloon-expandable valves with existing balloon-expandable valves and new self-expanding valves with existing self-expanding valves.