Robert Kormos
The US Food and Drug Administration (FDA) has granted Breakthrough Device Designation to Abbott for its in-development fully implantable left ventricular assist system (FILVAS). The FDA Breakthrough Device Designation programme will allow, according to Robert L Kormos (medical director for mechanical circulatory support at Abbott), the company to “fast track” the development of the new system. Specifically, the programme enables Abbott to have a prioritised interactive review with the FDA to help expedite the device’s development, and regulatory filing.
Speaking to BIBA Briefings, Kormos explains that the FILVAS will give people meaningful periods of time where they are completely untethered and have no external equipment to carry for four to six hours at a time. This is accomplished with an implanted battery and a system that can be charged across the skin, similar to the way a smartphone can be charged with a wireless charger. This could potentially lead to an improved quality of life for the patient.
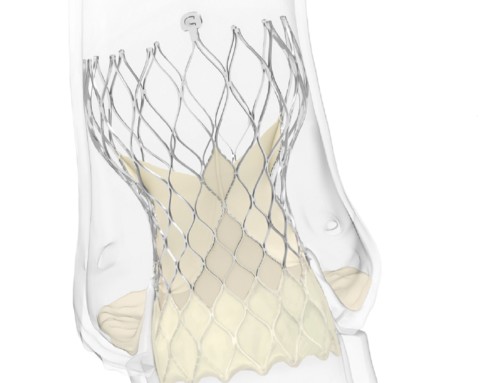
At present, LVADs are implanted into the body and then powered using an external battery pack or charging port. The other factor with the current systems, Kormos notes, is that you also have to wear the “brains”, or the controller, externally. “What we are aiming to do is have a fully implantable system, putting the controller and the battery inside the patient,” Kormos explains. He adds that having a system that provides patients “with a number of hours of support” before needing to be recharged means that they can be “free”. The need to wear an external battery and control system can seriously limit what patients are able to do. Thus, a fully implantable system may enable patients to be more mobile and even do activities. However, Kormos does note: “There is still a lot of development and testing required. The FDA Breakthrough Device Designation allows things to happen more efficiently.”
Speaking about the new FDA Breakthrough Designation, Michael Pederson, senior vice president for Abbott’s electrophysiology and heart failure division, states: “As the leader in heart failure management, a fully implantable heart pump has been our vision for the tens of thousands of people who progress into advanced heart failure each year. The potential for a fully implantable system would mean more freedom and a greater quality of life because there are no external components to be carried everywhere. These advances underscore Abbott’s long-standing commitment to develop innovative devices that allow those with heart failure to live their best lives.”
Less invasive approach
The granting of the FDA Breakthrough Device Designation to Abbott for the FILVAS follows on from the recent FDA approval for the device to be implanted via lateral thoracotomy—a surgical approach in which an incision is made between a patient’s ribs to access the heart. An Abbott press release states this technique has potential advantages over traditional open heart surgery because it can result in less bleeding and a shorter recovery time for patients.
The approval was based on two studies—the ELEVATE study (a multicentre, voluntary, observational registry collecting post-marketing data) and the LAT Feasibility study (a single-arm, prospective, multicentre study). According to the press release, the results of the two trials found that bleeding (requiring surgery), infection and arrhythmias were lower in the group implanted via lateral thoracotomy than those who underwent open heart surgery.
About this approval, Kormos says: “We continue to focus on advancing our heart failure devices and techniques to make life better for the patients we serve. The first approved LVAD—HeartMate I—was approved more than 25 years ago. Since that time, the technology has evolved immensely. Today’s HeartMate 3 device, including its design and size, allows physicians to successfully implant it without having to perform open heart surgery and offers two-year survival rates of 79%, as demonstrated in the MOMENTUM 3 clinical trial, comparable (82%) to that of heart transplants.”