Max Y Emmert
At the 2019 European Association of Cardio-Thoracic Surgeons (EACTS) annual meeting (3–5 October, Lisbon, Portual), Max Y Emmert (Institute for Regenerative Medicine, University of Zurich, Switzerland/the Department for Cardiothoracic and Vascular Surgery, German Heart Center Berlin and Charite Berlin, Germany) received the Techno-College Innovation Award for the LifeMatrix, a human cell derived acellular engineered tissue platform. The platform, potentially, could be used as material for cardiovascular implants, including transcatheter aortic valve implantation (TAVI) devices. Emmert, project leader of LifeMatrix at Wyss Zurich, talks to BIBA Briefings about the potential of LifeMatrix to address current challenges of existing implants.
What are the limitations of materials used for cardiovascular implants such as TAVI valves?
While transcatheter procedures have revolutionised cardiovascular medicine, the currently used prosthetic materials have not improved over the last decades and still lack the fundamental properties of human tissue. Specifically, they do not grow or regenerate, may cause infections and thrombosis, and, importantly, may have a limited durability and need replacing over time.
Transcatheter heart valves in particular are made from biological material of animal origin (bovine or porcine). These materials would normally cause an immunoreaction and, thus, be rejected. Therefore, the surface of these implants must be chemically modified. This, however, leads to continuous degeneration and calcification of the implant and negatively affects the durability of such implants.
Why might these limitations become more of an issue as transcatheter therapies move into younger/lower risk populations?
In line with what we have witnessed for surgical bioprostheses in younger patients, the implantation of a TAVI prosthesis into younger patients is expected to be associated with accelerated degeneration (compared with prostheses in older patients) that may require multiple reinterventions throughout the patient’s lifetime. And with every reintervention, the potential risk adverse events (i.e. procedural complications, infection, thrombosis, etc.) increases significantly. Such reinterventions may not only negatively affect the quality of the patient’s life but may also lead to increased costs for healthcare systems.
Tissue-engineered heart valves have already been developed to address some of these limitations. What historically have been the limitations of these valves?
The first attempts to cultivate a heart valve under laboratory conditions were made in the 1990s. The original idea was to grow a healthy heart valve in the laboratory with cells taken directly from the patient and then implant it back into the patient. This so-called autologous approach was widely used in tissue engineering and has been pursued by various research groups. But while this approach can work, it is a logistical nightmare that is associated with immense cost—meaning it is unlikely to become the standard of care. Therefore, the focus has now shifted towards in situ tissue engineering approaches with “off-the-shelf” concepts to enable clinical translation of such technologies.
What is the LifeMatrix solution?
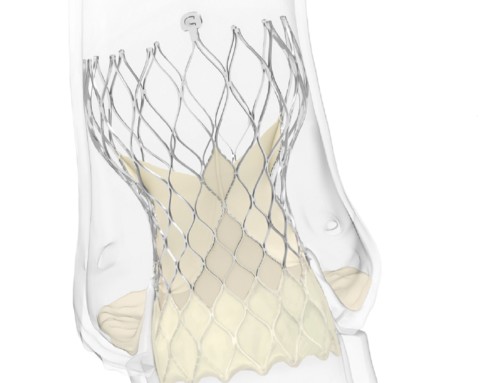
LifeMatrix has worked to transform classical autologous tissue engineering approaches into off-the-shelf implants. The implants have been designed to be manufactured as heart valves, blood vessels and other cardiovascular structures for both surgical and minimally invasive/transcatheter use. They are made from biodegradable polymer scaffolds and human cells (from Master Cell Banks and subsequently cultured in a bioreactor system) to create a human-cell derived extracellular matrix. Thereafter, the cells are removed, leaving behind an off-the-shelf product; one that is scalable, cost- effective, and non-immunogenic. The product is designed to be applicable to every patient. The idea is that the implant—which is cell-free at the time of implantation—will be repopulated by the recipient’s own cells and transform into living tissue. The goal is for it to grow and regenerate with the patient and, ideally, avoid the need for repeat interventions (and their associated risks).
What evidence is available for the LifeMatrix bioengineering platform?
The LifeMatrix biomimetic devices have undergone comprehensive preclinical testing showing feasibility, safety and efficacy for several indications. In particular, the preclinical development for a LifeMatrix Vascular Graft has been successfully completed. Several good laboratory practice (GLP) animal studies have been performed and have shown feasibility, safety, efficacy and growth capacity.
Also, the graft is currently being developed, in a clinical trial, for use as a cavopulmonary shunt in paediatric patients with single ventricle anatomy (Fontan procedure).
The safety and efficacy of the platform was also shown in the setting of transcatheter pulmonary heart valves (published in Science Translational Medicine in 2018). Using computational modelling inspired designs, such valves demonstrated clinical-grade performance together with native-like remodelling in a long-term translational sheep model. Furthermore, in vitro and in vivo studies have also demonstrated feasibility of the LifeMatrix TAVI device, which is currently in development.
What further trials are planned for the platform?
Since LifeMatrix is a true platform technology, hence additional indications in the cardiovascular space are under evaluation with a particular focus on congenital and structural heart disease.
Do you want to develop your own devices or do you want to sell the LifeMatrix platform to existing medical device companies for them to use?
Given the disruptive potential of the Lifematrix technology platform and that our main goal is to deliver next-generation implants with repair, remodelling and growth capacity to our patients, all options are being continuously explored!